Persistent Fatigue in Women: A Silent Signal of Insulin Resistance
Get Personalized Insights

Can chronic fatigue be resolved, or do I have to live with it for the rest of my life?
Fatigue is now one of the most common reasons women visit the doctor. More and more women between 30- and 45-years old report a specific set of symptoms. These include persistent tiredness that seems out of proportion to their workload, unexplained weight gain even though their eating habits haven't changed, and a drop in mental clarity.
Standard lab tests frequently come back as “within normal limits,” but women sense that something is not right. This collection of symptoms signals an early metabolic problem that can develop into chronic illness over the years. Detecting and correcting this metabolic imbalance is the key to resolving chronic fatigue and restoring energy levels
The metabolic explanation
The root-cause of chronic fatigue lies behind the energy-production mechanism of the body. Mitochondria are small power stations within our cells. Their job is to take glucose, the simplest form of sugar in the blood, and turn it into energy.
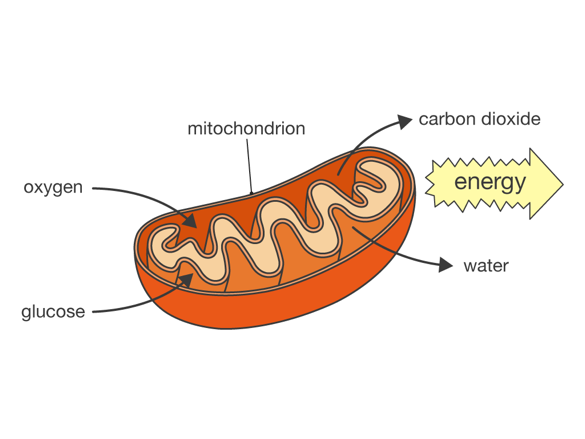
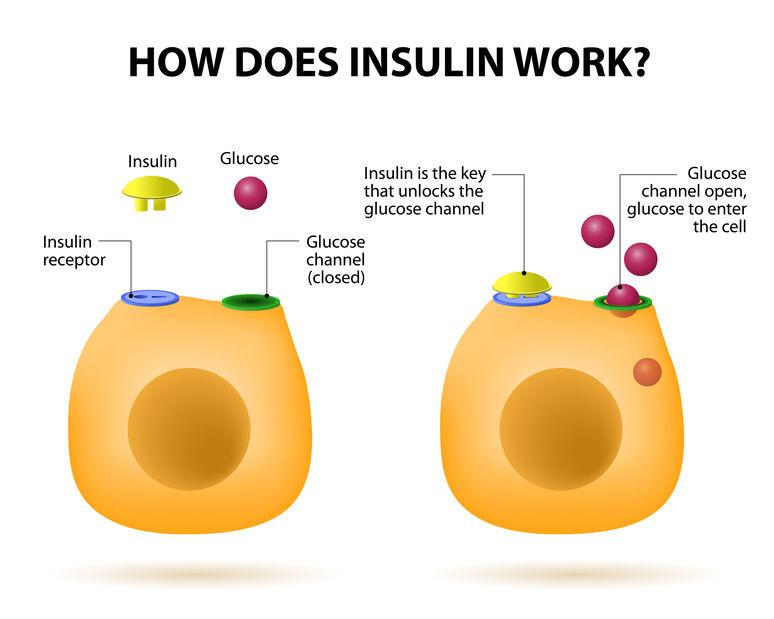
For this process to occur, glucose must first cross the cell membrane of cells. Insulin, a hormone released by the pancreas after we eat, controls this crossing. Insulin binds to on the cell surface, like a key fitting into a lock. This signal instructs the cell create a pathway for glucose to enter. Once inside, the glucose reaches the mitochondria, is broken down through a series of enzymatic steps, and ultimately produces energy.
Insulin resistance: what is it and why it matters
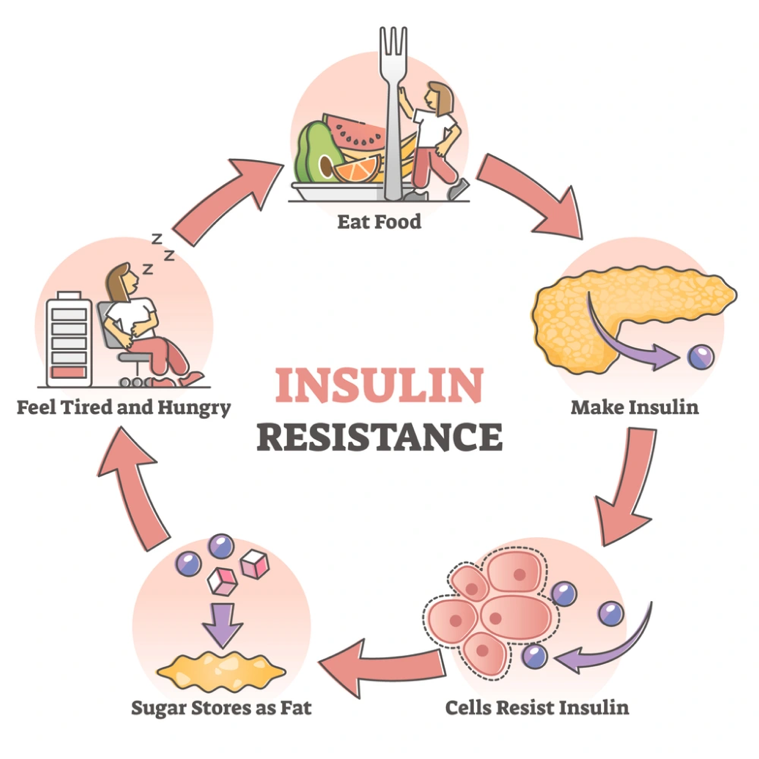
Under normal conditions, insulin binds to its receptor, opening the “gate” that allows glucose to enter muscle and liver cells. With insulin resistance, the gate does not respond properly. When cells fail to respond well to insulin, glucose cannot enter efficiently. As a result, glucose builds up in the blood, while mitochondria lack fuel. The paradox is clear: there is plenty of sugar outside the cell, but too little energy inside.
What is the primary factor contributing to insulin resistance?
In most cases, a chronic excess of circulating insulin drives the problem. This excess is triggered by repeated spikes in blood sugar. Diets rich in quickly absorbed carbohydrates, white bread, sweet drinks, and candy, make the pancreas release large amounts of insulin several times a day.
Over time, insulin receptors become less sensitive, much like how constant loud noise dulls hearing. Glucose then builds up in the bloodstream and causes more health issues. The extra glucose is stored as fat and damages the endothelial lining of blood vessels, increasing the risk of heart disease.
Visceral fat around the waist worsens the issue; it releases inflammatory molecules that disrupt insulin. Physical inactivity and ongoing psychological stress (cortisol), add more resistance.
Why the thirties and early forties are critical
Estrogen is the principal female sex hormone, synthesised mainly in the ovaries. Beyond its reproductive duties, it acts as a master regulator of metabolism, influencing how muscle and liver cells respond to insulin, how fat is stored, and even how the brain perceives appetite and satiety.
Estrogen typically improves insulin sensitivity. Events like pregnancy, the postpartum phase, and the beginning of perimenopause (mid 30s and early 40s) change estrogen levels and can cause metabolic instability.
Irregular sleep, work stress, and nutrient loss during menstruation can push the body toward insulin resistance. This increases the body’s demand for a lifestyle approach that prevents insulin resistance and promotes metabolic health.
Micronutrient gaps that intensify fatigue
The body needs more than 166 micronutrients to function (vitamins and minerals); these need to be present in sufficient amounts, and at the same time. A lack of any of those elements doesn’t allow metabolism to take place, thus impairing insulin sensitivity and energy production.
A healthy diet rich in vitamins provides the basis for the nutrients required. Nevertheless, due to modern agricultural methods, the content of fruits and vegetables in vitamins and minerals has decreased significantly in the last 60 years. This makes it more difficult for us to get all the necessary nutrients solely from the diet and deems supplementation necessary.
Iron, vitamin B₁₂, magnesium, and vitamin D are some of the most essential vitamins for mitochondrial energy production. Low levels of these nutrients, which are common in women due to insufficient intake from the diet, lack of supplementation, menstrual blood loss, and limited sun exposure, further reduce energy output. Addressing insulin resistance without correcting these deficiencies is like refuelling a car while leaving the battery dead.
Why routine blood work rarely finds the answer
Standard annual tests usually check only a few biomarkers including fasting glucose and HbA1c. Both can stay normal for years even after insulin resistance has started. A more useful assessment includes:
- Fasting insulin
- Uric acid
- HOMA-IR
- hsCRP
- A complete vitamin and mineral assessment (Iron, Ferritin, vitamin B₁₂, magnesium, vitamin D, calcium, omega 6:3)
Looking at these results alongside clinical symptoms helps develop a root-cause approach and a personalized intervention to restore insulin sensitivity and overall health.
Restoring physiological balance
To restore physiological balance and improve metabolic health, women should follow a personalized plan that addresses nutrition, supplements, and lifestyle. The best approach is to eliminate refined carbohydrates, processed foods, and excess sugar. A tailored supplement program should correct deficiencies and meet all micronutrient needs. Finally, lifestyle changes such as adding resistance training, quitting smoking, and reducing alcohol are essential for better metabolic health.
The KYMA Approach
At Kyma, we leverage personalized, evidence-based care to help women take control of their health. We use comprehensive blood testing, covering 100+ biomarkers, to pinpoint micronutrient deficiencies and metabolic dysfunctions. Our care team compiles a health plan unique for each client, which is centred around nutrition, supplements, exercise, and lifestyle. Additionally, we provide ongoing support through monthly health coaching sessions to ensure our customers get the care they need and feel empowered on their health journey.
Utilizing the power of technology, our team has created the Kyma online platform, which enables users to track their results over time and have all their health data in one place. Re-testing at 6 months helps you track your progress and adjust your plan where needed. Our goal is to help our customers understand exactly what’s happening inside their body and feel their best.
References
Ames, B.N. (2006). Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Proceedings of the National Academy of Sciences, 103(47), pp.17589–17594. doi:https://doi.org/10.1073/pnas.0608757103.
Dubey, P., Thakur, V. and Chattopadhyay, M. (2020). Role of Minerals and Trace Elements in Diabetes and Insulin Resistance. Nutrients, 12(6), p.1864. doi:https://doi.org/10.3390/nu12061864.
Kostov, K. (2019). Effects of Magnesium Deficiency on Mechanisms of Insulin Resistance in Type 2 Diabetes: Focusing on the Processes of Insulin Secretion and Signaling. International Journal of Molecular Sciences, 20(6), p.1351. doi:https://doi.org/10.3390/ijms20061351.
Maisel, P., Baum, E. and Donner-Banzhoff, N. (2021). Fatigue as the chief complaint. Deutsches Aerzteblatt Online, [online] 118(33-34). doi:https://doi.org/10.3238/arztebl.m2021.0192.
Maloney, E.M., Boneva, R.S., Lin, J.-M.S. and Reeves, W.C. (2010). Chronic fatigue syndrome is associated with metabolic syndrome: results from a case-control study in Georgia. Metabolism, 59(9), pp.1351–1357. doi:https://doi.org/10.1016/j.metabol.2009.12.019.
Naviaux, R.K., Naviaux, J.C., Li, K., Bright, A.T., Alaynick, W.A., Wang, L., Baxter, A., Nathan, N., Anderson, W. and Gordon, E. (2016). Metabolic features of chronic fatigue syndrome. Proceedings of the National Academy of Sciences, [online] 113(37), pp.E5472–E5480. doi:https://doi.org/10.1073/pnas.1607571113.
Shanahan, C. (2025). The energy model of insulin resistance: a unifying theory linking metabolic disease and cancer. Frontiers in Nutrition, 12. doi:https://doi.org/10.3389/fnut.2025.1532961.
Trimarco, V., Manzi, M.V., Mancusi, C., Strisciuglio, T., Fucile, I., Fiordelisi, A., Pilato, E., Izzo, R., Barbato, E., Lembo, M. and Morisco, C. (2022). Insulin Resistance and Vitamin D Deficiency: A Link Beyond the Appearances. Frontiers in Cardiovascular Medicine, [online] 9, p.859793. doi:https://doi.org/10.3389/fcvm.2022.859793.
Yan, H., Yang, W., Zhou, F., Li, X., Pan, Q., Shen, Z., Han, G., Newell-Fugate, A., Tian, Y., Majeti, R., Liu, W., Xu, Y., Wu, C., Allred, K., Allred, C., Sun, Y. and Guo, S. (2018). Estrogen Improves Insulin Sensitivity and Suppresses Gluconeogenesis via the Transcription Factor Foxo1. Diabetes, 68(2), pp.291–304. doi:https://doi.org/10.2337/db18-0638








.svg)
.svg)
.svg)